VEN Ethics Survey Results
Below are the overall de-identified results from our recent Ethics Survey for Vermont and New Hampshire conducted between July 15 and August 31, 2019. Questions that included identifying information about the respondent have been excluded from these publicly available results. For a more detailed analysis by audience type (e.g. Vermont hospitals, New Hampshire nursing homes, etc.), please contact us.
Respondent Demographics
- Total # of respondents: 172 (138 in Vermont; 21 in New Hampshire)
- Organizations represented:
- 24 hospitals (14 in Vermont; 10 in New Hampshire)
- 16 home health and hospice agencies (11 in Vermont; 5 in New Hampshire)
- 21 nursing homes (all in Vermont)
- 15 other organizations (8 in Vermont)
Respondent Characteristics
- Q: Is your organization designated a “Critical Access Hospital”?
- A: Yes: 31% / No: 61% / I don’t know: 8%
- Q: Have you ever served on an ethics committee?
- A: Yes: 52% / No: 48%
- Q: Have you ever received formal healthcare ethics training?
- A: Yes: 53% / No: 47%
- Q: Does your organization currently have an ethics committee?
- A: Yes: 64% / No: 27% / I don’t know: 9%
Issues Encountered
Q: In the following section, please think about how often you – or others in your organization – encounter ethical questions and conflicts in the areas listed:
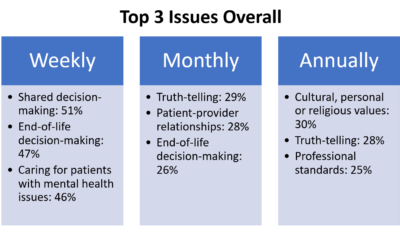
Summaries
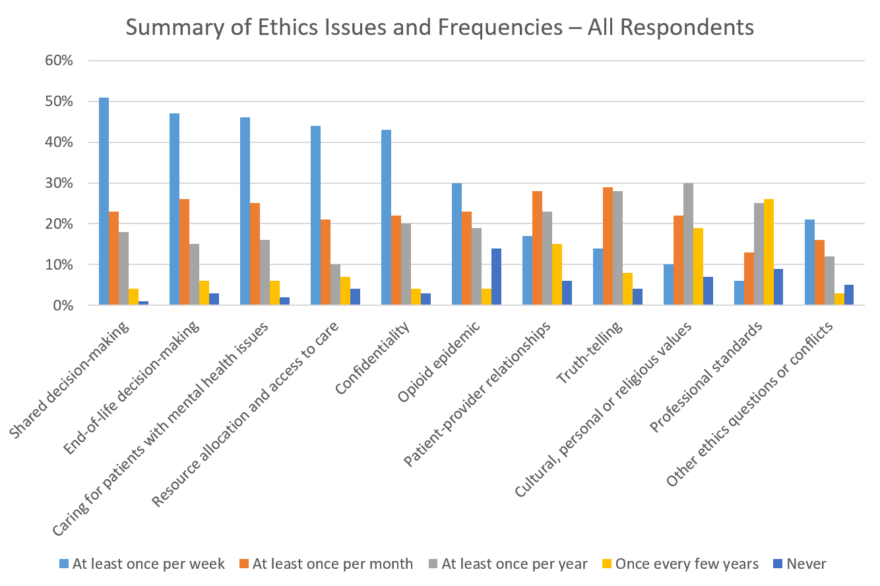
Full Data
| At least once per week | At least once per month | At least once per year | Once every few years | Never | I don't know | |
|---|---|---|---|---|---|---|
| Shared decision making, e.g. informed consent, determining patient decisional capacity/determining a surrogate, patient-family disagreements, requests for futile (non beneficial) treatments, etc. | 51% | 23% | 18% | 4% | 1% | 4% |
| End-of-life decision-making, e.g. questions about physician aid in dying, withholding or withdrawing life-sustaining treatment, code status discussions/advance care planning, health care proxy/surrogate decision-maker, etc. | 47% | 26% | 15% | 6% | 3% | 4% |
| Caring for patients with mental health issues, e.g. concerns over treatment plan, lack of appropriate placement or bed availability, stigma and/or bias affecting patient care, decision-making questions surrounding management of co-occurring psychiatric and somatic illness, etc. | 46% | 25% | 16% | 6% | 2% | 4% |
| Resource allocation and access to care, e.g. allocation of limited resources, inadequate staffing or services, difficulties creating equal access to healthcare, inability or refusal to pay for services, third party reimbursement issues, etc. | 44% | 21% | 10% | 7% | 4% | 13% |
| Confidentiality, e.g. privacy of patient information and records, boundary issues (relationships between patients and caregivers in the community), etc. | 43% | 22% | 20% | 4% | 3% | 8% |
| Opioid epidemic, e.g. staff distress in response to patient choices or behavior, stigma and bias affecting patient care, concern for under or over-treatment of pain, difficulty advocating for (or obtaining resources to provide) evidence-based care for patients using opioids, etc. | 30% | 23% | 19% | 4% | 14% | 10% |
| Patient-provider relationships, e.g. disagreement over plan of care, disclosure of conflicts of interest (financial incentives for research, treatments, or testing), legal conflicts (e.g. patient's right to refuse versus clinical obligations), etc. | 17% | 28% | 23% | 15% | 6% | 12% |
| Truth-telling, e.g. family decision-making or request to withhold information from a patient, disclosure of medical errors or adverse events, accurate and timely reporting of diagnosis and prognosis, etc. | 14% | 29% | 28% | 8% | 4% | 17% |
| Cultural, personal, or religious values, e.g. tension between local/cultural values and professional standards of care/institutional policy, clinician objection to treating a patient, patient refusal of standard of care, etc. | 10% | 22% | 30% | 19% | 7% | 12% |
| Professional standards, e.g. providing care outside scope of practice or evidence base, reporting peer impairment, reporting professionalism violations, etc. | 6% | 13% | 25% | 26% | 9% | 21% |
| Other ethics questions or conflicts not listed above | 21% | 16% | 12% | 3% | 5% | 43% |
Helpful Resources
Q: How helpful would additional ethics resources be in addressing ethical questions or conflicts in the following areas?
Summary
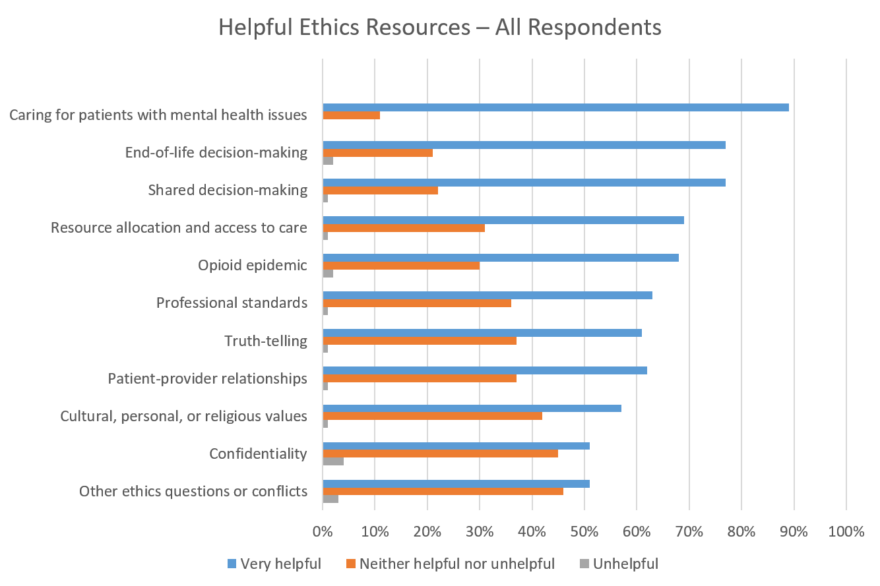
Full Data
| Very helpful | Neither helpful nor unhelpful | Unhelpful | |
|---|---|---|---|
| Shared decision making | 77% | 22% | 1% |
| End-of-life decision making | 77% | 21% | 1% |
| Confidentiality | 51% | 45% | 4% |
| Resource allocation and access to care | 69% | 31% | 1% |
| Truth-telling | 61% | 37% | 2% |
| Patient-provider relationships | 62% | 37% | 1% |
| Cultural, personal, or religious values | 57% | 42% | 1% |
| Professional standards | 63% | 36% | 1% |
| Opioid epidemic | 68% | 30% | 2% |
| Caring for patients with mental health issues | 89% | 11% | 0% |
| Other ethics questions or conflicts not listed above | 51% | 46% | 3% |
Q: Which of the following resources would help staff address clinical ethics issues more effectively at your organization?
Summary
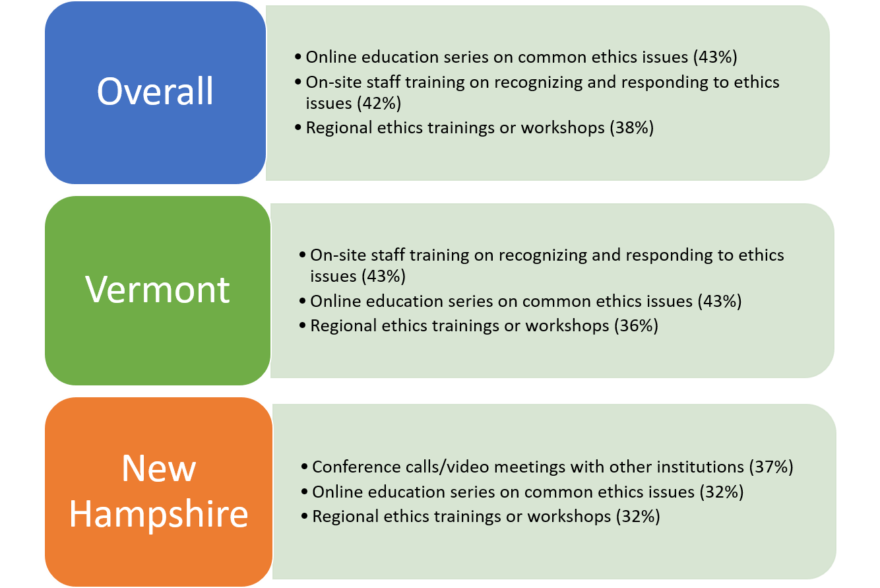
Full Data
| Currently available; additional resources are not needed | Currently available; additional resources would be helpful | Currently unavailable; additional resources are not needed | Currently unavailable; additional resources would be helpful | I don't know | |
|---|---|---|---|---|---|
| Online education series on common ethics issues (audio/video) | 7% | 27% | 11% | 43% | 13% |
| On-site staff training on recognizing and responding to ethics issues | 12% | 32% | 8% | 42% | 6% |
| Regional ethics trainings or workshops | 9% | 36% | 10% | 38% | 7% |
| Conference calls/video meetings with other institutions involving discussions of recent cases | 10% | 24% | 13% | 35% | 18% |
| Online or print healthcare ethics resources that address common ethical themes and guide staff in responding to ethics issues | 13% | 38% | 5% | 32% | 13% |
| Help developing written polices for addressing ethics issues | 13% | 24% | 13% | 25% | 25% |
| Access to clinical ethics consultation (on-site/in-person) | 26% | 36% | 7% | 21% | 9% |
| Local ethics committee | 31% | 38% | 4% | 15% | 12% |
Collaboration Opportunities
Q: Please rate your interest in collaboration with the following types of established ethics programs or services:
Full Data
| 1 (Not Interested) | 2 | 3 | 4 | 5 (Very Interested) | |
|---|---|---|---|---|---|
| State-wide ethics organizations | 3% | 8% | 20% | 29% | 40% |
| Local, multi-facility partnerships | 4% | 10% | 19% | 28% | 39% |
| Academic medical centers | 7% | 10% | 23% | 34% | 26% |
| All of the above | 2% | 8% | 22% | 29% | 40% |
Opportunities for Improvement
Q: Please select the 3 greatest opportunities to improve ethics quality in your organization:
Summary
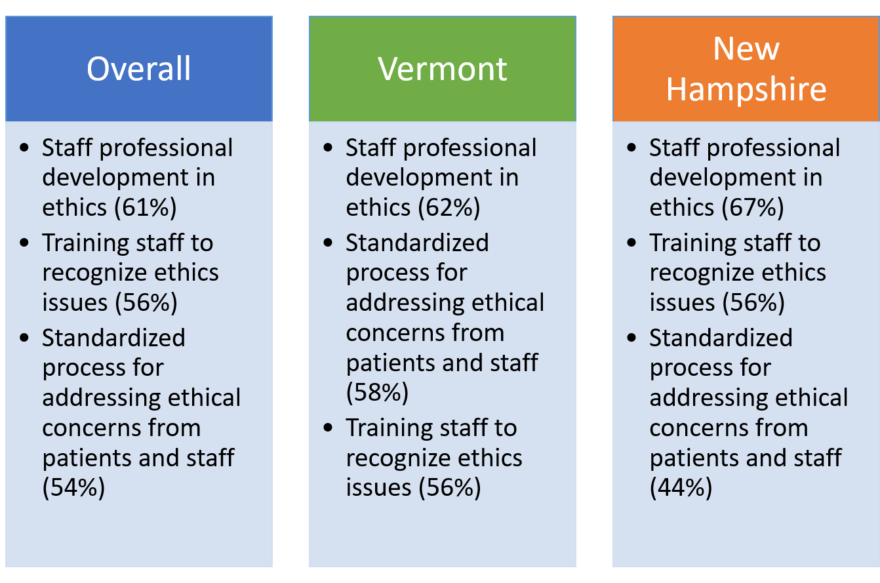
Full Data
| Choice | Response |
|---|---|
| Staff professional development in ethics | 60% |
| Training staff to recognize ethics issues | 56% |
| Standardized process for addressing ethical concerns from patients and staff | 54% |
| Determining the role of ethics in the organization | 33% |
| Ethics policy development | 26% |
| Leadership support of staff who raise ethical concerns | 26% |
| Concern about impacting relationship with the community | 15% |
| I do not know enough about existing quality gaps to answer | 9% |